NEWS
OAGS Case of the Month
Hosted by OAGS President Dr. Ravinder Singh.
Follow on social media channels.
Scroll down for previous case outcome summaries.
Unable to see the case below? Click here. Conversation/results: download
Dr. Singh will share his previous case outcome here after a new one is posted each month.
December Case of the Month Recap
15 year old female presents to ER with what seems like an infected Bartholin Cyst. She is seen and assessed by Gynecology and taken to the OR for an I&D. Intra-operatively during the EUA, the gynecologist also feels an abnormality on the anterior aspect of the rectum: inflammation and granulation; pus draining from an opening. What advice would you give the Gynecologist?
1. CT abdomen/pelvis to ensure no collection, Antibiotics, and outpatient colonoscopy.
2. MRI pelvis, Antibiotics, and outpatient colonoscopy.
3. Antibiotics and outpatient colonoscopy
4. Refer to GI
Actual Care Outcome:
This patient had a CT scan prior to discharge to ensure there was no collection/abscess; results: no abscess; thickening of the rectum. She was sent home with antibiotics and then had a colonoscopy as an outpatient that confirmed Crohn’s Disease. An MRI pelvis is pending as she had abnormal drainage from her vagina; and she was referred to GI and Colorectal surgery.
Conversation/results: download
September Case of the Month Recap
77 year old Male who was referred for a colonoscopy because of FIT +ve. He also had a FMHx of a 1st degree relative with colon cancer. But, this patient had never undergone a colonoscopy. Colonoscopy findings: cecal cancer, multiple adenomas, and a large upper rectal adenoma with extensive high grade dysplasia on pathology. Staging CT confirmed cecal cancer and no other local-regional or distant disease. CEA was normal. What would you do next?
- 1. Right Hemicolectomy with shorter interval flexible sigmoidoscopy/colonoscopy
- 2. Right Hemicolectomy + Anterior Resection
- 3. Sub-total Colectomy with ileo-rectal anastomoses
June Case of the Month Recap
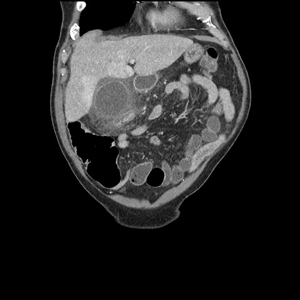
A 33 year old Male obese but otherwise no systemic co-morbidities. Two year history of biliary colic and previous episode choledocholithiasis requiring ERCP. Got lost to follow-up over that 2 year period and didn’t get a cholecystectomy. Presented with cholangitis and required a repeat ERCP, sphincterotomy, and stent. Went on to have a sub-total cholecystectomy. No drain was left in-situ. Returns POD#5 with fevers, abdominal pain, and elevated WBC. He was admitted and put on IV ABX. CT image below. What would you do next?
1. IR Drainage
2. Surgical Drainage
3. Repeat ERCP and stent placement
4. Refer to HPB
Due to it being a weekend when he presented and he was getting septic, he was taken to the OR for a Laparoscopic Drainage of the biloma and peritoneal washout, and wide drainage. He went on to have a repeat ERCP and longer stent placed. He did well and was discharged home with outpatient follow-up with respect to the drain.
Conversation/results: download

A 35 Female with cervical cancer and left sided fluid collection with drain. She underwent a loop ileostomy and clinically got better. But unfortunately, follow-up CT showed a new mesenteric mass. She is seeing oncology in hopes of getting chemo- and immunotherapy (has positive markers sensitive to immunotherapy). Hoping if she responds, she can perhaps be considered for surgical resection or remain on palliative immunotherapy.
Original Case Query:
A 35 Female otherwise healthy was diagnosed with cervical cancer. She underwent TAH + BSO. Based on pathology she did not need adjuvant treatment. She developed recurrence at the vaginal cuff and then received radiation. Post-radiation, she developed intra-abdominal collections on the right and left side of the abdomen. The right one spontaneously resolved but the left persisted. A drain was inserted and cytology/cultures were sent. The cytology was negative initially and culture showed Gram Positive bacteria. Repeat cytology was done due to the lack of resolution of the collection and subsequently it showed cancer cells. Drain eventually started draining stool. What would you do? CT provided.
1. Upsize drain: radiologically or surgically
2. Refer to Surgical Oncology
3. Left Hemicolectomy with or without anastomoses
4. Loop Ileostomy
Results: download
Poll Results/Feedback: download
Original Case Query:
A 16 year old female with history of obesity presented with several day history of abdominal pain. CT showed acute appendicitis. She was taken to the OR and she had significant inflammation in the RLQ with sigmoid and ileum adhered to what was presumed to be the area of the appendix. She had a small abscess that was drained but further dissection was impossible. A JP drain was placed and she was kept on ABX. Folllow-up CT revealed a decrease in inflammation and no abscess; the drain was removed and she was booked for an interval appendectomy. Intra-operatively, she had less inflammation but had dense adhesions. The appendix was removed. Pathology revealed a T4N0 NET (NeuroEndocrine Tumour) at the tip 8mm in size. Of course she was M0 based on 2 CT scans. What would you do next?
1. PET scan
2. NET Metabolic work-up
3. Refer to Neuroendocrine Specialty Clinic
4. Right Hemicolectomy
Poll Results: download
Original Case Query:
82 Male with a PMHx of Atrial Fibrillation on anticoagulation, and a pacemaker. Presents with upper abdominal pain, nausea, and vomiting. This has been periodic over the last several months but worse in the last several days. Otherwise stable. Blood work ok. CT scan is as follows: sludge in the gallbladder; no biliary dilatation; LFTs normal.
What would be your management?
a. Antibiotics alone and reassess need for cholecystectomy at a later date
b. Antibiotics and Cholecystostomy (after NOAC is held for 48-72h)
c. Antibiotics and Cholecystectomy (after NOAC is held for 48-72h)
d. Send to HPB
Case outcome will be shared with next month’s case!